Airborne Diseases: an Overview
Airborne diseases come in many forms and range in severity, but there’s one thing that aids in combating them all: knowledge. Arm yourself with information on airborne disease types, symptoms, prevention, and more.
The following is for informational purposes. Please seek professional medical advice should you require medical assistance or medical care.
What Is an Airborne Disease?
Airborne diseases are diseases that you can catch merely by breathing. These diseases are spread when those who are infected sneeze, cough, talk, or even exhale, releasing throat and nasal secretions into the air.
While the diseases can then land on and contaminate surfaces, they can also hang in the air, so that others nearby — including both humans and animals — can inhale them and become infected.
Airborne diseases tend to spread more easily than other types of diseases, and, thus, are harder to control.
What Are The Common Types of Airborne Diseases?
Numerous airborne diseases exist, and some are continually mutating (or adapting), such as the viruses that cause the common cold. Some of the most common airborne diseases include:
- COVID-19: The rapidly spreading novel coronavirus, COVID-19 first appeared at the end of 2019 and soon caused a global pandemic. Scientists and the medical community are still learning more about COVID-19 and information is being updated accordingly. Common symptoms of COVID-19 include shortness of breath, cough, fever, and fatigue.
- Influenza: Most people have had the flu at one point or another, as it spreads easily and becomes contagious before symptoms are even apparent. It continues to be contagious for another week or so — potentially longer if you have a weakened immune system. The many different strains of the flu and its ability to mutate make it difficult for people to develop immunity, necessitating annual flu vaccinations.
- The common cold: More often than not, when people get sick and can’t make it to work or school, it’s because of the common cold. Most adults get a cold two or three times a year, and children get them even more often, adding up to one million cases of the common cold in the U.S. every year. The majority of these cases are caused by a rhinovirus, although many different viruses can cause colds.
- Mumps: Mumps are very contagious and can be spread before symptoms appear and for as long as five days afterward. Once quite common in the U.S., mump cases have declined by 99% thanks to vaccinations and now occur mostly in densely populated areas. The Centers for Disease Control & Prevention (CDC) reported 70 U.S. cases in January 2020.
- Chickenpox: Caused by the varicella-zoster virus, chickenpox takes up to 21 days to develop after exposure and can be spread for one to two days before a rash appears. Most people can only get the chickenpox once, but it sometimes reactivates later in life as a painful skin condition known as shingles. Those who have never had the chickenpox before can contract the disease from someone with shingles.
- Measles: Measles is highly contagious, as the virus that causes it can remain active on surfaces or in the air for up to two hours, and it’s transmissible for up to four days before and four days after a rash appears. In 2018, 140,000 people died from measles, which is also the leading cause of death among children worldwide. Luckily, most people only contract the measles once. The measles vaccine prevented an estimated 23 million deaths between 2000 and 2018. A total of 1,282 measles cases were reported in 2019 in the U.S., where the disease occurs mostly in unvaccinated people.
- Tuberculosis (TB): Also referred to as “consumption,” TB is an airborne bacterial infection but doesn’t spread easily, requiring long periods of close contact with an infected person. It’s possible to contract TB without giving it to other people or becoming ill: While 1.4 billion people worldwide have TB, only about 10 million of those cases are active. The group with the greatest likelihood of developing the disease are people with weakened immune systems. Symptoms may appear within days or take as long as months or years to appear, but once the disease activates, the bacteria rapidly multiply, attack the lungs, and spread to other organs, bones, and skin through the bloodstream and lymph nodes.
- Whooping cough: Pertussis, commonly known as the whooping cough, causes the airways to swell and manifests as a relentless hacking cough. It’s most contagious during the first two weeks after the cough appears. About 24.1 million whooping cough cases are seen every year, causing 160,700 deaths. 15,609 whooping cough cases were reported in the U.S. in 2018.
- Diphtheria: Diphtheria injures the respiratory system and can cause damage to the nerves, kidneys, and heart. It was once a leading cause of sickness and death in children but is now rare in the U.S. due to widespread vaccination (the past decade has seen fewer than five reported cases). Worldwide, about 7,100 cases of diphtheria were reported in 2016.
Common Symptoms of Airborne Diseases
Common cold and flu symptoms are typical of many airborne diseases. These symptoms include:
- Sneezing
- Coughing
- Stuffy or runny nose
- Sore throat
- Congestion
- Sinus pressure
- Fatigue
- Chills
- Body and muscle aches
- Headaches
- Low fever
- General sluggishness
Diagnosis for Airborne Diseases
Diagnosing an airborne disease is usually accomplished through a saliva sample, involving a throat swab. Your doctor may also want to take blood tests or analyze other bodily fluids.
Prevention for Airborne Diseases
While complete prevention is impossible for airborne diseases, people can reduce their exposure to the pathogens that cause them using:
- Vaccines: Vaccines have been crucial in reducing the infections and deaths caused by airborne diseases and are the best way to protect both yourself and others. Vaccinations exist for the measles, chickenpox, mumps, and the flu. A vaccine for COVID-19 is currently in development.
- Hygiene: Good hygiene is important to prevent the spread of all infectious diseases, including practices such as washing your hands often, sneezing and coughing into your mouth or a tissue, and staying home when you’re sick. However, airborne diseases require additional measures, since you can easily inhale them if you’re within 6 feet of an infected person. Try to maintain at least 6 feet from others anytime you’re in a public place.
- Ventilation: Proper ventilation is key to prevent the spread of airborne diseases. Modern hospitals use high-quality ventilation systems, but simpler measures can also be effective in residential environments. For example, open windows and doors, clean and maintain your home’s ventilation system regularly, and consider adding special filters to promote airflow.
- Masks: While the CDC does not recommend that people routinely wear masks outside of the health care setting to avoid contracting the seasonal flu, they have changed their guidelines for the recent COVID-19 outbreak. People should wear masks or face coverings in public places where other social distancing measures are difficult to maintain, such as grocery stores.
Treatment for Airborne Diseases
Speak with your doctor as soon as you begin experiencing systems of an airborne disease to begin treatment. Treatment will vary depending on the type of airborne disease, but may include:
- Symptom management: Your doctor may recommend that you manage your symptoms with over-the-counter medications. For example, over-the-counter pain relievers such as acetaminophen may help with sore throat, body aches, and fever. Cold and cough medications can also be helpful to manage symptoms of airborne diseases, but should be used with caution, especially when paired with other medications.
- Rest: Plenty of rest is required to recover from airborne viruses. Stay home from work or school and get a lot of sleep.
- Prescription medications: Antiviral medications may be prescribed in some cases, such as to shorten the severity and duration of a flu infection. Your doctor may also prescribe antibiotics in severe cases to prevent secondary infections such as pneumonia. Your already weakened immune system is especially susceptible to secondary infections, which can sometimes become even more dangerous than the airborne disease itself.
More serious airborne diseases — such as COVID-19 and whooping cough — may require hospitalization.
Airborne Isolation Precautions
When hospitalization is necessary to treat an airborne disease, the CDC requires that the infected patient be placed in airborne isolation — the strictest level of its transmission-based precaution guidelines. The CDC has specifically mandated airborne isolation for patients who have contracted influenza, COVID-19, Middle East respiratory syndrome (MERS-CoV), severe acute respiratory syndrome (SARS-CoV), and Ebola.
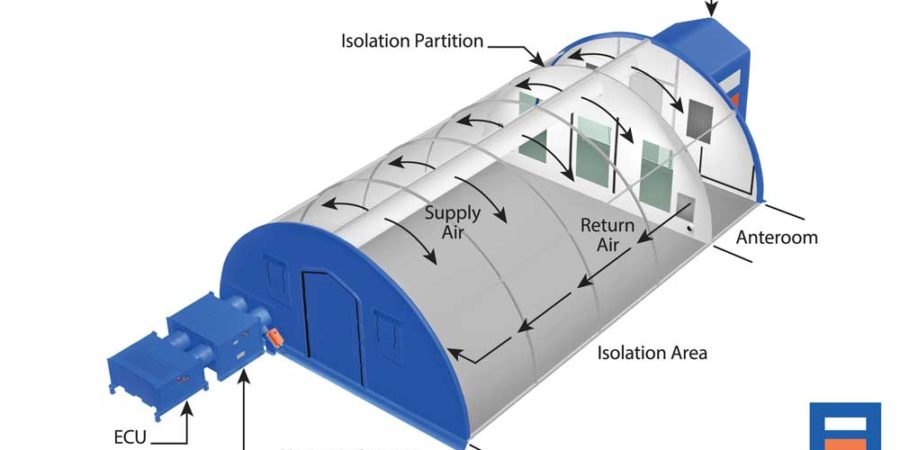
Airborne isolation typically involves placing patients in isolation rooms known as “negative air pressure rooms” or “negative pressure isolation rooms,” in which a specialized filter system removes the air and prevents it from flowing into other spaces. These isolation rooms must have a closed door, and medical staff must wear specialized respirator masks when they enter the space.
Why Use A Negative Pressure Isolation Rooms From BLU-MED?
When outbreaks of airborne diseases occur, government agencies and health care organizations need to be ready to slow its spread and treat infected patients immediately. Rapidly deployable negative pressure isolation shelters from BLU-MED Response Systems® are crucial to any swift and effective response.
BLU-MED medical shelters equipped with negative pressure isolation systems exceed the requirements for Airborne Infection Isolation (AII) and manage the three elements of indoor air quality (particles, biologicals, and gaseous volatile organic compounds [VOCs]). These medical shelters can be used on their own or easily scaled to create isolation wards and mobile hospitals.
What’s more, the shelters can be set up in as little as 30 minutes, are designed to endure snow loads of up to 20 PSF and wind gusts of up to 100 MPH, and can support both short- and long-term isolation and quarantine operations.
Organizations across the nation are currently using BLU-MED isolation shelters to treat patients infected with COVID-19 and stop the spread of this airborne disease. For availability and delivery options, contact us at +1-425-739-2795 or inforeq@blu-med.com.