Guide to Creating Space for Medical Surge
The novel coronavirus known as COVID-19 has been an eye-opener for hospitals around the nation and the world that did not have the infrastructure to accommodate such a sudden increase in demand. Faced with patients in need of urgent care and nowhere to treat them, hospitals in outbreak epicenters have had to get creative: One hospital in New York has even lined the hallways of the emergency department with patient beds and hung plastic sheets from the walls with duct tape to separate off coronavirus isolation areas.
This sudden spike in demand and hospitals’ ability to meet it is known as “medical surge,” and because no one can predict when emergencies such as the coronavirus will occur, governing health care organizations recommend that hospitals prepare for medical surge in advance. Depending on the level of demand and existing resources available, this preparation may involve plans for implementing temporary surge sites to expand hospital infrastructure.
But as this recent outbreak has shown us, creating space for medical surge is complicated, and involves tactical considerations regarding the types of structures to use, how to implement and manage them, and more.
This guide is for informational purposes only. If planning a temporary medical surge site, we recommend contacting your state or country’s governing agencies for specific health and safety standards.
What Is Medical Surge?
According to the Public Health Emergency site from the U.S. Department of Health & Human Services, medical surge refers to health care organizations’ (HCOs’) ability to provide adequate medical evaluation and care during times that exceed the limits of the community’s normal medical infrastructure. In response to events such as mass casualties or infectious diseases, HCOs must exhibit medical system resiliency by maintaining or rapidly recovering any compromised operations.
Medical surge encompasses both medical surge capacity and medical surge capability, collectively referred to as MSCC.
Medical Surge Capacity
Medical surge capacity specifically involves the ability to evaluate and care for a spike in patient volume that stresses or exceeds normal operating capacity.
While most strategies to address medical surge capacity focus on identifying additional resources such as hospital beds, equipment, supplies, pharmaceuticals, and personnel, successful plans should first consider the ability to maximize current resources. Creating management systems and processes to govern asset use is also crucial.
Medical Surge Capability
Medical surge capability, on the other hand, is the ability to manage patients who require highly specialized or unusual medical evaluation and care, including issues that require intervention to protect other patients and health care providers. Medical surge capability requirements encompass specialized medical services such as personnel, equipment, procedures, information, and expertise that aren’t normally available at a given location.
Examples in which medical surge capability comes into play include instances of highly infectious diseases, such as the severe acute respiratory syndrome (SARS) outbreak in 2003 and the current COVID-19 global pandemic. The high transmissibility of the illnesses makes caring for them challenging, requiring protections for and regular screening of staff and other patients.
Medical Surge Capacity and Capability Management
Health care organizations may not be able to prevent the types of events that provoke medical surges, but they can certainly take steps to prepare for them and mitigate their negative effects. Keep in mind that medical surge isn’t the responsibility of the emergency department, but of the entire hospital, including both in-patient and out-patient services.
All hospitals should have an emergency operations plan as well as tactics for implementing this plan whenever usual strategies no longer meet patient demand. This plan should address four components: space, supplies, staff (the resources that will be necessary), and systems (the processes, procedures, and policies that will govern the allocation and conservation of those resources).
This guide is concerned with the first of the resources. Health care organizations can create space for medical surge using either internal surge options or temporary surge sites.
Internal Surge Options
Internal surge plans consist of hospitals’ strategies to increase their ability to manage a surge of patients internally, without the use of additional sites. Sometimes referred to as “surging in place,” these strategies should be part of every emergency operations plan.
The U.S. Department of Health & Human Services’ Technical Resources, Assistance Center, and Information Exchange (TRACIE) recommends the following internal surge tactics:
- Discharge patients early when possible and use discharge holding areas.
- Keep clinics open during evenings and weekends to prevent patients from going to the emergency room (ER).
- Transition patients to care in observation areas when possible.
- Cancel elective procedures to save beds for ER admissions.
- Open additional units or beds that are closed but licensed.
- Convert private rooms into semi-private rooms that can accommodate more than one patient.
- Review patient care plans to identify patients whose care plan could be adapted to accommodate a different room.
- Use geri-chairs instead of full beds when possible, such as for short-term observation admissions and administering bronchodilators, hydration, and similar treatments.
- Cancel classes and training to increase staff availability.
- Use teaching staff and supervisors to provide direct patient care.
- Flex staff to changing needs.
Temporary Surge Sites
When internal surge options aren’t sufficient to meet patient demand, health care organizations must also turn to temporary surge sites, or “surge hospitals.” Surge hospitals encompass any facilities designed to supplement existing hospitals in the case of an emergency and can serve as space for waiting rooms, triage, isolation, treatment, and more.
Health care organizations, their communities, and local governments should work together to plan for what kinds of surge hospitals to use and how to implement them in advance in order to expedite care if the need for medical surge arises.
Types of Surge Hospitals
No standard model or plan for surge hospitals exists. Instead, health care organizations must assess their options and make their choice based on their community’s needs and the resources available to them.
The Joint Commission on Accreditation of Healthcare Organizations identifies the following types of surge hospitals:
- Closed wards or shuttered hospitals: The Agency for Healthcare Research and Quality (AHRC), a branch of the U.S. Department of Health & Human Services, recommends using closed hospitals to expand surge capacity during two occasions: instances of mass casualty and outbreaks of infectious diseases that require quarantines to prevent transmission. Ideally, the shuttered hospital or ward should be thoroughly assessed as a viable option in advance as part of the organization’s emergency preparedness plan. Whether the closed hospital/ward is identified in advance or as an urgent response to an emergency, it needs to be inspected and cleaned by an environmental crew to ensure that the air, water, and overall environment are safe and sanitary before anyone else enters the space.
- Facilities of opportunity: Nonmedical community buildings that are within close proximity to a medical center, of the appropriate size, and available for temporary use are considered “facilities of opportunity” that can be adapted into surge hospitals. Facilities of opportunity could include exhibition halls, convention centers, airport hangars, sports arenas, hotels, veterinary facilities, schools, empty warehouses, and the like. The easiest sites to adapt are medical facilities designed for other purposes, such as surgery centers. By designating specific buildings as surge hospitals and equipping them for patient overflows, health care organizations can prepare themselves for emergencies without having to purchase additional facilities.
- Mobile medical facilities: Mobile medical facilities are another option for surge hospitals, and include unique building solutions such as an 18-wheeler truck equipped with surgical and intensive care units. These units generally have six beds, pre-op and post-op recovery areas, siloed utility rooms, and a central nursing station. While these facilities are beneficial in that they can be used as portable clinics when not needed for disaster management, their principal drawback is the need for a large area to store them when not in use.
- Portable medical facilities: Portable, mobile medical facilities are self-contained turnkey systems that come fully equipped with medical supplies and equipment. These facilities can be set up and ready to use in just a few hours to provide urgent care as soon as possible. When no longer needed, they can easily be disassembled and stored for future use.
Triggers and Thresholds for Temporary Surge Sites
Triggers and thresholds indicating when to activate surge sites will vary from one facility to the next, and could be based on factors such as emergency department volume, inpatient volume, or lack of flex space. Every facility should identify their triggers and thresholds in advance and make sure all facilities across the hospital understand them for a unified response.
Regulatory and Legal Considerations for Temporary Surge Sites
Under normal circumstances, temporary surge sites may be used on or within a hospital’s campus as long as they meet all the conditions of participation for the Centers for Medicare and Medicaid Services (CMS) and comply with county and state life safety code requirements and licensure.
However, during federal-level emergencies, the Secretary of Health and Human Services can temporarily modify or waive certain Medicare, Medicaid, HIPAA, or CHIP requirements using section 1135 of the Social Security Act (called “1135 waivers”). These waivers make it easier for health care providers to give beneficiaries the care they need during an emergency.
Contact your county and state government for information on local legal regulations related to temporary surge sites. For information on waivers and flexibilities during the coronavirus pandemic, visit the CMS website.
Operational Considerations for Temporary Surge Sites
Health care organizations should take these considerations into account when deciding to implement a temporary on-site surge facility:
- Demand length: How long will the temporary surge site be necessary for? Consider whether the length of demand warrants the time it will take to set up the facility. Portable medical facilities are a great option to ensure quick and easy setup.
- Cost: Will it make more financial sense to rent or purchase a structure, considering the potential for repeated long-term use if you buy it? If you rent, consider the potential additional costs if you need to keep the structure for longer than anticipated. If you purchase, consider long-term maintenance costs.
- Optics: Be ready to manage community expectations and patient perceptions. Patients may be concerned about receiving inferior care in a surge hospital, especially if the facility consists of low-quality structures. If using a portable or mobile medical facility, consider choosing an option that has been deployed successfully during past emergencies by well-known organizations to give patients peace of mind.
- Location: Make sure that the location you’ve chosen for the surge hospital can accommodate the footprint of both the facility and its associated equipment, and that the facility comes with anchoring options that are compatible with the intended location. Especially if you’re using modular structures, have a plan in place for extreme weather, such as electrical storms, high winds, and snow. Finally, if you plan on purchasing a facility instead of borrowing, consider modular scalability and configuration potential with existing assets. This would allow your organization to expand the facilities or potentially combine them with other equipment in future emergency situations.
- Capabilities: Determine what capabilities are available in the surge facility you’re considering and, if any crucial capabilities are lacking, whether you’ll need to limit the kind of care you can offer there. Key capabilities include:
- Power — determine if:
- Power supply will come from a generator or electrical connections.
- There are enough charging stations.
- Lighting is available both inside and outside the surge site.
- Climate control
- Laboratory capabilities (such as point-of-care urine, point-of-care blood, urine pregnancy, rapid strep and influenza, and blood glucose tests)
- IV fluids / lab draws
- Oxygen
- Radiology services
- Electrocardiography (ECG)
- Suction
- Crash cart
- Positive/negative airflow areas
- Pharmaceuticals — ensure:
- A safe location for medications
- On-site medications
- Ability to get other/additional medications from the emergency department or a pharmacy
- Space layout — ensure:
- Sufficient number of beds
- Sufficient storage space
- Ability to store frequently used items (such as extra masks and gloves) on-site
- Sufficient space for staff to sit and complete charting
- Restrooms
- Ability to protect patient privacy
- Ability to prevent cross-infection/cross-contamination
- Computer, IT, and biomedical technology access
- Overhead paging
- Hospital radio and phone reception
- Personal protective equipment (PPE)
- Handwashing and hand sanitizer dispensers
- Equipment graded for austere environments
- Laundry bins, sharps containers, biohazard receptacles, and trash cans
- Chairs for visitors in the treatment area
- Geri-chairs, beds, or elevated beds for patients
- Power — determine if:
Deactivating Temporary Surge Sites: Returning to Baseline Capacity & Capability
Deactivation is the final step of managing medical surge capacity and capability. Although deactivation may require less urgency than the original response, health care organizations should still have plans set for deactivation in advance. Make sure to take the following steps when planning for deactivation:
- Determine triggers for closing the temporary surge site.
- Determine how long your facility can qualify as a “temporary site,” as regulations may apply after a certain point (oftentimes 30 days).
- Notify your organization’s partners and relevant authorities.
- Complete inventory on equipment and supplies:
- Restock any supplies that came from your regular inventory.
- Replenish any supplies that came from your disaster cache and prepare for storage.
- Return any surge site supplies to their original locations for future use.
- Turn off your electronic medical records’ (EMRs’) surge module.
- Clean the surge site thoroughly.
- If using a portable medical facility, disassemble and store the structure(s) for future use.
- Review your organization’s MSCC management to identify areas for improvement and lessons learned.
Hospital Surge Facilities From BLU-MED
For health care organizations that are interested in establishing a long-term solution for managing medical surge capacity and capability, BLU-MED Response Systems® sets the standard for hospital surge facilities and rapidly deployable medical shelters.
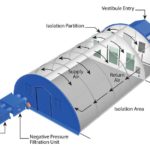
BLU-MED’s fully equipped turnkey mobile medical facilities can serve as space for patient overflow, triage, surgery, extended care, emergency rooms, intensive care units, and more to help hospitals meet isolation and surge capacity — including mass casualty requirements. These facilities are designed for use as category C isolation units (negative pressure isolation rooms) to help limit the risk of infecting or contaminating medical staff, patients, and hospital buildings. The CDC requires the use of negative pressure isolation rooms to treat patients infected with infectious airborne diseases such as COVID-19.
BLU-MED’s hospital surge facilities are also:
- Rapidly deployable: Setup for one medical shelter takes as little as 30 minutes for a trained group of four. Forkliftable and reusable containers make the medical shelters easy to store when not in use and to transport when needed at a new site.
- Scalable: Because BLU-MED’s surge facilities are modular, they can easily be configured to meet immediate needs and then reconfigured or expanded later as those needs change. Sizes range from 650 square feet for a single structure to 65,000 square feet for an entire mobile field hospital.
- Electrical-equipped and climate-controlled: BLU-MED surge hospitals are integrated with UL-tested lighting, electrical, HVAC, and a specialized five-ton environmental control unit (ECU) that maintains a comfortable interior temperature of 65 to 75 degrees F even in extreme weather conditions.
- Durable: Surge facilities from BLU-MED are engineered to withstand 100-mph winds, snow loads of 20 pounds per square foot, and heavy rain, so you can rest assured that they’ll outlast the duration of the emergency.
- Tested and proven: BLU-MED’s mobile hospital solutions are designed to meet the U.S. military’s exacting standards and have been proven in combat operations and extreme climates around the globe. We have experience creating rapidly deployable military shelter systems for mid-to-long-term operations in harsh and remote locations.
The U.S. Air Force Expeditionary Medical Support (EMEDS) program, U.S. Army Combat Support Hospitals, U.S. Air Force BEAR program, and U.S. Special Operations Command Joint Bare Base program use BLU-MED solutions exclusively. - Backed by support services: BLU-MED also offers disaster response training and exercise services, and manages inventory by maintaining equipment, replenishing supplies, and repackaging. All of the following organizations have utilized BLU-MED’s support services:
- U.S. Air Force
- U.S. Army
- U.S. Special Operations Command
- U.S. Navy
- U.S. Marine Corps
- National Guard
- UK Ministry of Defense
- United Nations
- FEMA
- Red Cross
- DMAT
- Air National Guard
- Northwest FEMA Team (Pierce County Search and Rescue, WA)
Health care organizations, emergency management services, government agencies, and nongovernmental organizations (NGOs) around the world have relied on BLU-MED’s mobile hospital facilities and portable medical shelters to meet their medical surge needs. For more information on how our solutions can help your own organization, contact us online, email us at inforeq@blu-med.com, or call us at +1-888-680-7181 (+1-425-739-2795 for international customers).