Preparing for the Potential Return of COVID-19
The question of whether a second wave of the novel coronavirus known as COVID-19 will occur is no longer up for debate. Now scientists are considering what that return may look like, and three potential scenarios have emerged — all of which require hospitals to prepare to scale their facilities both short- and long-term.
A Second Wave of COVID-19
Since the coronavirus outbreak was first declared a pandemic, scientists have been warning about the likelihood of a second — and much worse — wave of infections. History supports their predictions: The second waves of the Spanish flu pandemic in 1918-1920 and the H1N1 epidemic in 2009-2010 were both particularly devastating.
These warnings are sounding once more as governments around the world begin to ease lockdown restrictions.
Dr. Andrea Ammon, director of the European Centre for Disease Prevention and Control (ECDC), points out that around 85 to 90% of the population is still susceptible to the disease. When asked about the possibility of a second wave of infections, she says that it’s no longer a question of if a return may occur, but of “when and how big.”
Epidemiologists are asking themselves the same question, with varying results. The University of Minnesota’s Center for Infectious Disease Research and Policy (CIDRAP), a global leader in emerging infectious disease response and public health preparedness, recently released an analysis that outlines three possible scenarios — none of which involves a quick return to normal:
- Scenario 1: A series of continual smaller waves occur throughout the summer of 2020 and then every few months for the next one to two years. These waves would alternate with periods of only a few cases and would gradually diminish sometime in 2021. Location, social distancing measures, and social distancing relaxing would all likely influence the severity of these waves. Mitigation measures may need to be reinstituted and relaxed intermittently over the one- to two-year period.
- Scenario 2: This scenario most closely resembles scientists’ original predictions: COVID-19 returns in a larger wave in the fall or winter of 2020, followed by one or more smaller waves in 2021. (This pattern is similar to what occurred during the 1918-1919, 1957-1958, and 2009-2010 pandemics.) Mitigation measures would be necessary once more in the fall to reduce the spread of the disease and avoid overwhelming health care systems.
- Scenario 3: A “slow burn” of consistent cases and transmission (represented on a graph by ripples without a clear wave pattern) follows the first wave of COVID-19 through the end of 2022. Like scenario 1, this pattern may fluctuate by location depending on the level of mitigation in place. While strict mitigation measures would probably not need to be reinstituted in this scenario, new cases and deaths would continue as the new normal.
Whichever route the pandemic takes, one thing is clear: COVID-19 won’t be going away in 2020 — and maybe not even in 2021. While a vaccine would drastically influence these timelines, the epidemiologists behind the study don’t predict a vaccine to be available until sometime in 2021 at the earliest, and that is notwithstanding any obstacles that could cause delays during vaccine development.
Preparing Health Care Systems for the Second Wave
The one benefit of knowing with certainty that a second wave of coronavirus will occur is that there’s time to prepare — either to continue with previous or current mitigation measures or to implement different or stronger tactics. To that end, the CIDRAP analysis issued several recommendations in addition to its potential scenarios:
- Health authorities should plan for the worst-case scenario (the second scenario above), including no herd immunity or vaccine.
- Health care organizations and government agencies should work to ensure adequate protection for health care workers as the second wave begins.
- Government officials should develop specific triggers and plans for reinstituting mitigation measures.
- Government officials should make it clear to the public that they need to be prepared for COVID-19 to resurge over the next one to two years.
In both its outlining of the potential scenarios and these recommendations, CIDRAP emphasizes the importance of preparedness for health care organizations, particularly to prevent their infrastructures from becoming overwhelmed. While mitigation measures can help to slow disease spread and prevent a sudden spike in cases, CIDRAP suggests that health care organizations prepare for the worst, which entails a much larger peak than occurred in spring 2020.
For many health care organizations, preparing will mean ensuring a sufficient staff of health care professionals to treat the infected, personal protective equipment (PPE) for these workers, and adequate space, beds, and medical equipment for proper treatment. Amesh Adalja, an emerging diseases expert at the Johns Hopkins University Center for Health Security, points out that many hospitals will take advantage of the summer “to manage capacity better and make adjustments to be better able to absorb a surge of cases,” having now seen the disastrous consequences of being ill prepared.
Medical Structures for Changing Needs
But while hospitals can contract additional staff and stockpile masks, ventilators, and other medical equipment with time, coming up with additional space may prove more challenging — especially if we end up having a bad flu season this coming fall.
The dilemma is not only how to find more space to treat COVID-19 patients without encroaching upon other hospital facilities, but also a question of how much space and for how long it will be necessary. Depending on which scenario plays out, hospitals may need to plan for:
- A slight scaling of facilities over the next two years (scenario 1)
- A drastic scaling of facilities this fall (scenario 2)
- Significant scaling over the next two years due to continual new outbreaks (scenario 3)
While CIDRAP recommends that hospitals prepare for the worst (scenario 2), hospitals would likely do well to consider and be ready for any of the above situations. For many hospitals and health care organizations, finding a solution to all three of these possibilities will mean investing in and relying upon rapidly deployable medical facilities.
Organizations such as University Medical Center in El Paso, Texas, Grand Strand Regional Medical Center in Myrtle Beach, South Carolina, and the University of Utah Health have already relied on BLU-MED Response Systems® (BLU-MED) modular medical shelters to help get them through the first wave of COVID-19. With versatile functionality, rapid deployment, the durability necessary for long-term use, and the ability to be disassembled and stored in between outbreaks, these modular hospital facilities are an ideal solution to meet changing, unpredictable needs.
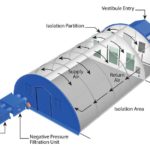
Whether your organization is ready to start preparing for the second wave of COVID-19 or you merely want to start thinking through your response options, reach out to BLU-MED today. We can review the benefits of a deployable field hospital or deployable morgue system to meet medical surge, a negative pressure isolation system (NPIS) to quarantine infected patients, or a custom facility to meet your specific needs.
Being a division of Alaska Defense, leading provider of military shelter systems, we have the experience to provide mobile hospital solutions that ensure a safe, clean environment conducive to advanced-level care in any climate for extended periods of time.
For more information about BLU-MED call us at +1-(888)-680-7181, email inforeq@blu-med.com, or fill out the online inquiry form on our contact page.