COVID-19 Vaccinations Can Prevent Hospital Surges
Since COVID-19 vaccines were released in the spring of 2021, 70.4% of the United States population has received at least one dose, according to the Centers for Disease Control and Prevention (CDC). Getting close to three-quarters of the population almost fully immunized should be a reason to celebrate.
However, in spite of the country’s rising vaccination rates, new COVID cases in hospitals are continuing to rise due to Delta variant infections among the unvaccinated. And once again, patient surges are pushing hospitals to capacity.
[Related: Airborne Diseases: An Overview]
Increased Hospitalizations From Unvaccinated Patients
CNN states, “For the first time since February, more than 50,000 hospital beds across the country were occupied by Covid-19 patients, according to new data from the US Department of Health and Human Services. That number is more than triple what it was a month ago.”
With more than half of the U.S. population still not fully vaccinated, and more than 90 million people without a first dose, the healthcare system is under immense pressure — more so than when COVID first wreaked havoc in early 2020.
As of August 4, the seven-day vaccination average is 446,300, which is the highest it has ever been. However, health experts say this rate needs to be much higher.
Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, hopes to see the nation’s vaccination rates reach one million or more per day to lower the nation’s new infection rates and get COVID-19 under control.
In order to avoid hospital surges in the coming winter months, it’s absolutely vital that more Americans become fully vaccinated to help the country and their relevant communities heal, while potentially saving their own lives, too.
[Related: COVID-19 Delta Variant Raising Concerns and Hospitalizations]
COVID-19 Variants Cause Wave of New Cases
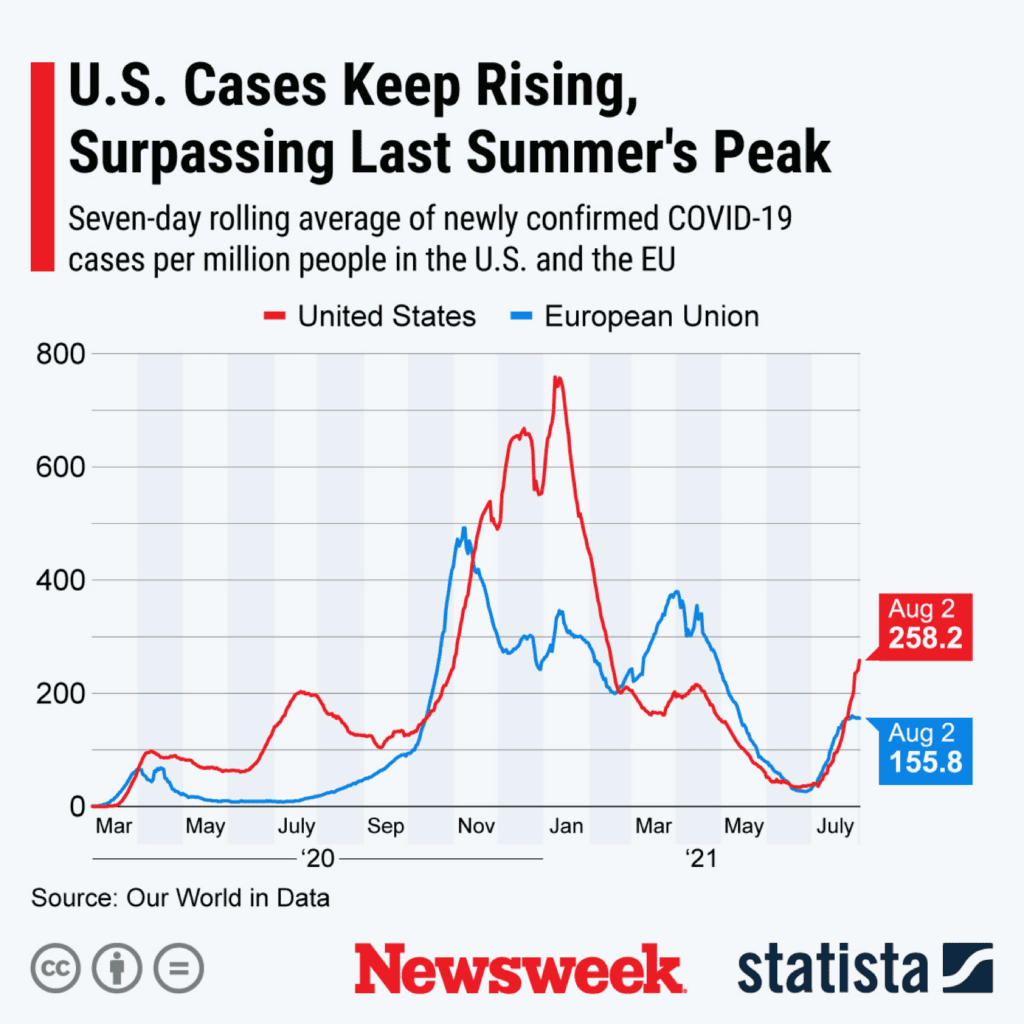
Experts believe that a fourth wave of COVID will hit the nation if safety measures are lifted and high numbers of Americans remain unvaccinated.
According to data from the CDC, the Delta variant has now accounted for 93.4% of new COVID-19 cases. The numbers reveal evidence that getting vaccinated works and will prevent potentially life-threatening symptoms.
New case rates are even higher in select states, such as Iowa, Kansas, Missouri, and Nebraska, as well as many of the sunbelt states, including Florida, Georgia, Alabama, Mississippi, Louisiana, and Texas.
The former U.S. Surgeon General, Dr. Jerome Adams, explained in an interview with the Washington Post, “We are not crying wolf here. This surge that we’re going through right now has every potential to be — and already looks to be — the worst surge we’ve faced so far.”
[Related: Preparing for the Potential Return of COVID-19]
COVID Surge Is Straining Florida Hospitals
With numbers this high, hospitals are quickly becoming overwhelmed. And when capacities are soon reached, many ill or dying patients could be turned away.
Florida, which has the most unvaccinated people in the nation, is the record-setter for the country’s highest number of new cases in one day: 16,935 hospitalizations were recorded on August 3, making it the third consecutive day Florida has topped its own record.
The Sun-Sentinel noted 50,997 new COVID-19 cases and 100 deaths over the previous three days. Florida has now had the highest number of cases since the start of the pandemic a year and a half ago and accounts for 21.3% of new COVID cases in the U.S.
Since high infection rates are causing patient surges, emergency rooms are once again growing more crowded by the day.
The President of the Florida Hospital Association, Mary Mayhew, told MSNBC, “Last year, in 2020 it took us 60 days to go from 2,000 cases to 10,000. It has taken us 27 days to break our 2020 peak so it has been a dramatic increase.”
Many hospitals in Florida are forced to convert existing spaces such as conference rooms, auditoriums, and cafeterias into isolation wards in an effort to efficiently utilize staff. But since these makeshift wards aren’t standard medical best practice, the exits, entryways, and floor layouts cause safety concerns due to patient proximity, ultimately putting nurses, physicians, and hospital personnel at an increased risk of infection.
Other hospitals in Florida are setting up medical tents and mobile field hospitals, such as those from BLU-MED Response Systems® (BLU-MED), capable of providing negative pressure systems and hospital surge facilities for safe isolation and treatment.
[Related: Key Elements of Pandemic-Ready Healthcare Facilities]
New Cases of COVID and Rising Hospitalizations in Texas
Texas also has one of the highest infection rates in the nation and ranks at No. 36 for its amount of fully vaccinated people.
Like in Florida, the Delta variant has caused Texas hospitals to fill up quickly.
While the original COVID-19 strain primarily affected elderly people, those between the ages of 18 and 49 are seeing the most hospitalizations nationwide from the Delta variant. In Texas, low vaccination rates among younger crowds mean that the ages of hospitalized patients are even lower, with those in their 20s and 30s requiring breathing machines and other intensive care treatment.
As of August 2, more than 52,000 Texans have died from COVID-19, and the vast majority were unvaccinated. According to The Texas Tribune, “COVID hospitalizations in Texas quadrupled in July. Preliminary data from the state indicates that more than 99.5% of people who died due to COVID-19 in Texas from Feb. 8 to July 14 were unvaccinated.”
14 million Texans remain unvaccinated.
[Related: Antibody Infusion Centers for COVID-19]
New and Highly Contagious COVID Variants Emerging
Based on variant classifications from the World Health Organization (WHO), emerging virus variants are either a Variant of Concern (VOC) or a Variant of Interest (VOI).
VOCs are more contagious than original strains, more fatal, and more resistant to vaccines and treatment therapies.
VOIs are a SARs CoV-2 variant that has the genetic evolutionary capability to affect certain factors of the virus, such as immune strength, symptom severity, contagion levels, and treatment success. VOIs are especially threatening to public health worldwide.
The Alpha, Beta, Gamma, and Delta variants are classified as VOCs, and the Eta, Iota, Kappa, and Lambda variants are VOIs.
While the nation’s focus and efforts are currently on the Delta variant, health experts are becoming increasingly concerned about the Lambda variant.
Lambda was first identified in Peru, accounting for 50% of positive tests in Lima in March of 2020. By April, Lambda was found in 80% of positive tests. A 30% increase in transmission within a single month is extremely concerning.
As of August 3, 1,037 cases of the Lambda variant were reported in the U.S.
Health experts think that Lambda may be more resistant to antibodies that are induced through vaccination, and may possibly cause high rates of breakthrough infections.
Regardless, getting vaccinated and continuing to follow safety protocols such as social distancing and wearing a mask are the best protection you can take against COVID-19 at this time.
BLU-MED Medical Shelters Can Lessen the Impact of Patient Surges
For more information about BLU-MED or our negative pressure rooms and mobile field hospitals and medical shelters, call us at +1-(888)-680-7181, email inforeq@blu-med.com, or fill out the online inquiry form on our contact page.
Featured image via Wikimedia Commons


